Spinal Surgery
Spinal Surgery
We are well qualified to offer surgical treatment of disorders affecting the whole spine extending from the neck to the lower lumbar spine. This includes the management of degenerative disorders in the cervical, thoracic and lumbar spine (disc herniation, spinal stenosis, myelopathy, spondylolisthesis), fractures and dislocations at all levels of the spine, deformity (scoliosis and kyphosis) and infections in the spine.
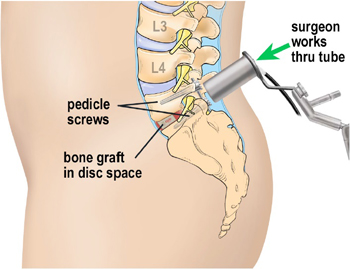
Minimally Invasive Spine Surgery Treatments ( MISS )
Minimally invasive spine surgery (MISS) is sometimes called less invasive spine surgery. In these procedures, doctors use specialized instruments to access the spine through small incisions.
Minimally invasive spine surgery was developed to treat spine problems with less injury to the muscles and other normal structures in the spine. It also helps the surgeon to see only where the problem exists in the spine. Other advantages to MISS include smaller incisions, less bleeding, and shorter stays in the hospital.
Spine surgery is typically recommended only when a period of nonsurgical treatment — such as medications and physical therapy — has not relieved the painful symptoms caused by your back problem. In addition, surgery is only considered if your doctor can pinpoint the exact source of your pain, such as a herniated disk or spinal stenosis
Vertebroplasty or kyphoplasty
Vertebroplasty or kyphoplasty may be a treatment option if you have painful vertebral compression fractures from:
- Osteoporosis (a depletion of calcium in bones)
- Metastatic tumor (cancer spread from another area)
- Multiple myeloma (cancer of the bone marrow)
- Vertebral hemangioma (benign vascular tumor)
You may not be a candidate if you have:
- Non-painful stable compression fractures
- Bone infection (osteomyelitis)
- Bleeding disorders
- Allergy to medications used during the procedure
- Fracture fragment or tumor in the spinal canal
Vertebroplasty and kyphoplasty will not improve old and chronic fractures, nor will they reduce back pain associated with poor posture and stooping forward. Traditional treatment used to involve waiting 4 to 6 weeks to see if patients improved on their own, but now it’s believed that waiting allows the bone to harden, making vertebroplasty or kyphoplasty less effective. Many doctors are now suggesting vertebroplasty as soon as the first week after a fracture for some patients because the results are significantly better
Microscopic Spine Surgery
Microscopic discectomy is the most common surgical treatment for ruptured or herniated discs of the lumbar spine. When the outer wall of a disc, the annulus fibrosus, becomes weakened, it may tear allowing the soft inner part of the disc, the nucleus pulposus, to push its way out. This is called disc herniation, disc proplapse or a slipped or bulging disc. (See discussion of herniated disc for more information.) Once the inner disc material extends out past the regular margin of the outer disc wall, it can press against very sensitive nerve tissue in the spine. The disc material can compress or even damage the nerve tissue, and this can cause weakness, tingling or pain in the back area and into one or both legs. Open discectomy uses surgery to remove part of the damaged disc and thus to relieve the pressure on the nerve tissue and alleviate the pain. The surgery involves a small incision in the skin over the spine, removal of some ligament and bone material to access the disc and the removal of some of the disc material.
Open discectomy has been performed and improved over the course of the past 60 years. Over time, the procedure has been refined, and improved diagnostic tools—such as magnetic resonance imaging (MRI) and computerized tomography (CT) scans—have allowed physicians to gain a better understand of which patients will have the best results from the surgery.
Who is a Candidate?
Not all patients with herniated discs are candidates for the open discectomy procedure. Most people find pain relief with nonsurgical treatments such as rest, physical therapy, anti-inflammatory medications and epidural injections. However, sometimes the pain does not respond to these therapies and may require a more aggressive intervention.
If back and leg pain does not respond to nonsurgical treatment and continues for four to six weeks or longer, the physician may prescribe diagnostic tests, such as X-ray imaging, MRI or a CT scan, to verify the source of the pain. If a diagnosis of herniated disc is confirmed, open discectomy may be recommended.
The Procedure
Microscopic (Open) discectomy is usually performed under general anesthesia (the patient is unconscious) and typically requires a one-day hospital stay. It is performed while the patient is lying face down or in a kneeling position. During the procedure, the surgeon will make an approximately one-inch incision in the skin over the affected area of the spine. Muscle tissue is removed from the bone (lamina) above and below the affected disc and retractors hold the muscle and skin away from the surgical site so the surgeon has a clear view of the vertebrae and disc. In some cases bone and ligaments may have to be removed for the surgeon to be able to visualize and then gain access to the disc without damaging the nerve tissue. This is called a laminectomy or laminotomy depending on how much bone is removed.
After the Procedure
After surgery, you may feel pain at the site of the incision, and the original pain may not be completely relieved immediately after surgery. Your doctor may prescribe pain medication to ease you through the immediate postoperative period. You will be instructed on deep breathing techniques and encouraged to cough in order to free your lungs of any fluid buildup that may occur due to the general anesthesia. It is recommended that, with supervision, you begin walking as soon as you are fully recovered from the anesthesia. This will aid in your recovery.
Before you are discharged from the hospital, a physical therapist may visit with you to help you feel comfortable performing activities such as climbing stairs, sitting and getting out of a car or bed. Once you are discharged from the hospital, your physician may prescribe a physical therapy regimen suited to your condition.
At home, you may have some minor restrictions such as not sitting for long periods of time, lifting objects more than five pounds, or excessive bending or stretching for the first four weeks after surgery. Also, you should not attempt to drive an automobile until you have been instructed to do so by your physician.
